Meeting local needs
As a trusted partner to all stakeholders, we are committed to delivering equitable health outcomes and improving access to care for all communities.

Health equity
At Arataki PHO we believe healthcare should be accessible, equitable and designed for patients and their whānau.
Equity is woven into everything we do - from how we deliver care, to the partnerships we form, to the way we monitor our impact. Our focus is on helping to eliminate inequities, particularly for Māori, Pacific peoples, and communities who experience barriers in access, experience, and outcomes.
Models of care
Arataki PHO is committed to removing barriers and making healthcare accessible to everyone:
- Multiple care options: In-person consultations and nationwide 24/7 online care.
- Inclusive care: The Tend app is available in te reo Māori, and our clinicians speak a wide range of languages.
- Proactive care: Targeted recalls, health promotion initiatives, and high care needs models to support patients to stay well.
Partnerships and people
Equity cannot be achieved alone. We partner with iwi and Māori organisations to deliver services aligned with whānau needs and aspirations.
We are dedicated to building a workforce that reflects our communities. This includes:
- Actively recruiting and supporting Māori and Pasifika health professionals.
- Providing ongoing training in health equity and cultural safety for all staff.
- Supporting patient choice by publishing clinician languages, specialty interests (e.g. Māori health, rainbow health, women’s health), and cultural expertise via the Tend app and website.
Data and monitoring
Accountability is central to our approach. Our Outcomes Framework aligns with the Government Policy Statement on Health and the NZ Health Plan, ensuring we track and report on health equity outcomes.
Outcomes framework
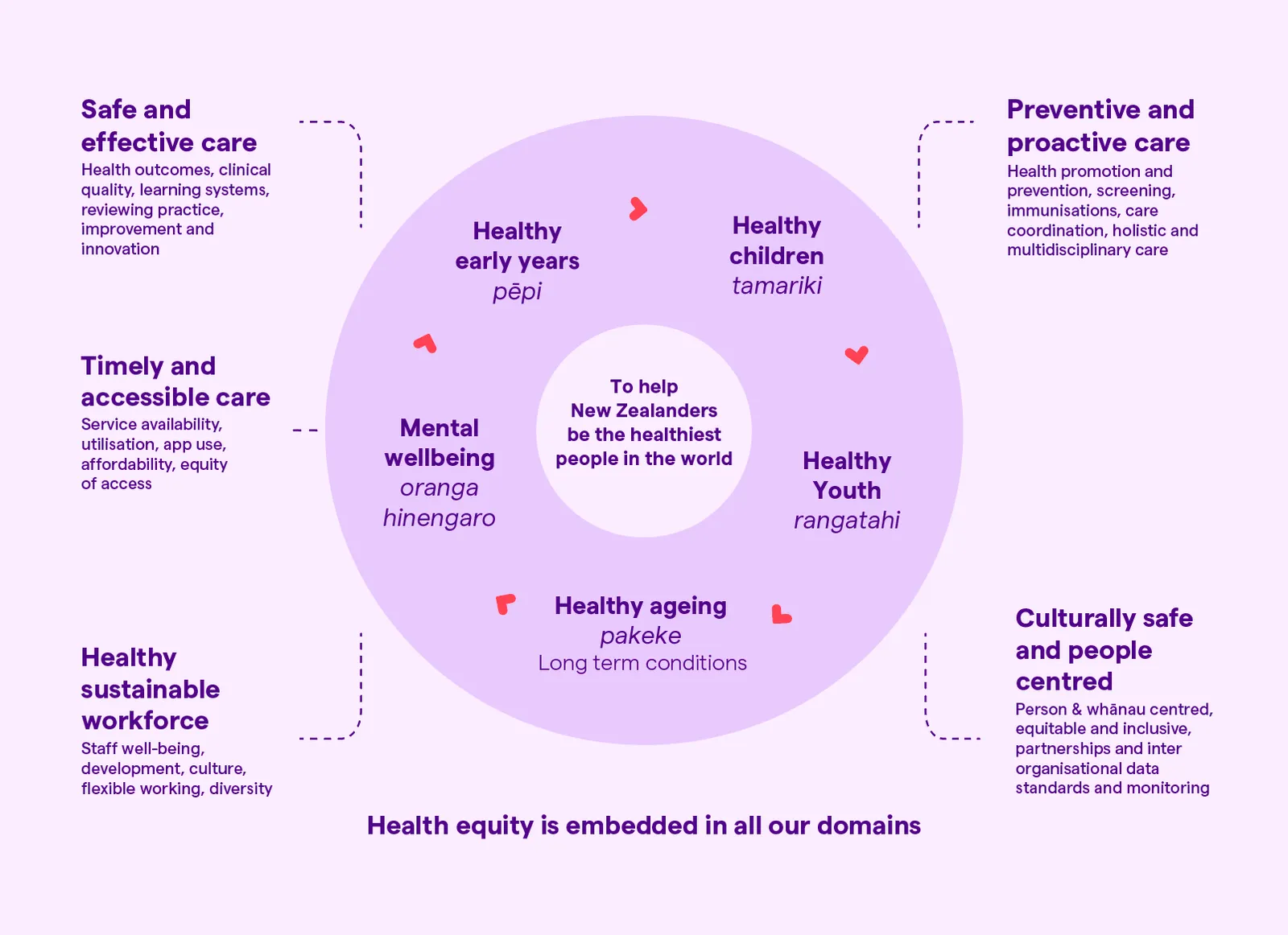
Equity indicators
We currently monitor more than 30 clinical and equity indicators across key domains
Long-term condition management
- HbA1c control
- Cardiovascular risk assessments (CVRA)
- Cardiovascular disease management outcomes
- Diabetes management and timely reviews
Preventative care
- Immunisation rates across the life course
- Screening participation and follow-up
- Smoking cessation advice support
Timely access
- Appointment wait times
- Online and in-person service utilisation
- ED presentations (impact of primary care on hospital load)
- Repeat prescription turnaround times
Safe and effective care
- Adverse events
- Antibiotic stewardship
- Controlled drug prescribing
Culturally safe and people-centered care
- Patient reported outcomes
- Enrolment rates by ethnicity
- Satisfaction metrics
- Workforce diversity
All indicators are stratified by ethnicity and high-needs populations to identify inequities and drive targeted improvement. We are also developing new indicators to strengthen reporting on mental wellbeing and workforce wellbeing.
Health outcomes
Connecting with communities
Beyond digital engagement and in-clinic care, Arataki PHO is committed to community-based outreach to improve health literacy, service accessibility and engagement with under-served populations.
This includes taking part in events like Big Gay Out, where we provide on-site health promotion initiatives to support Rainbow communities. We’ve also supported Hitting For Hearts, a charity golf event raising awareness about heart health and the importance of not ignoring early signs. In addition, we’ve partnered with Ngāti Whātua Ōrākei to deliver accessible health checks for their whānau, helping to promote early detection and preventative care within the community.
Targeting care through data-driven insights
Our data-driven approach identifies high-needs populations to support targeted health initiatives such as care management, immunisation campaigns and early intervention. Central to this is our High Care Needs Model, so care is aligned with each patient’s medical complexity, promoting better outcomes for those with chronic or complex health conditions.
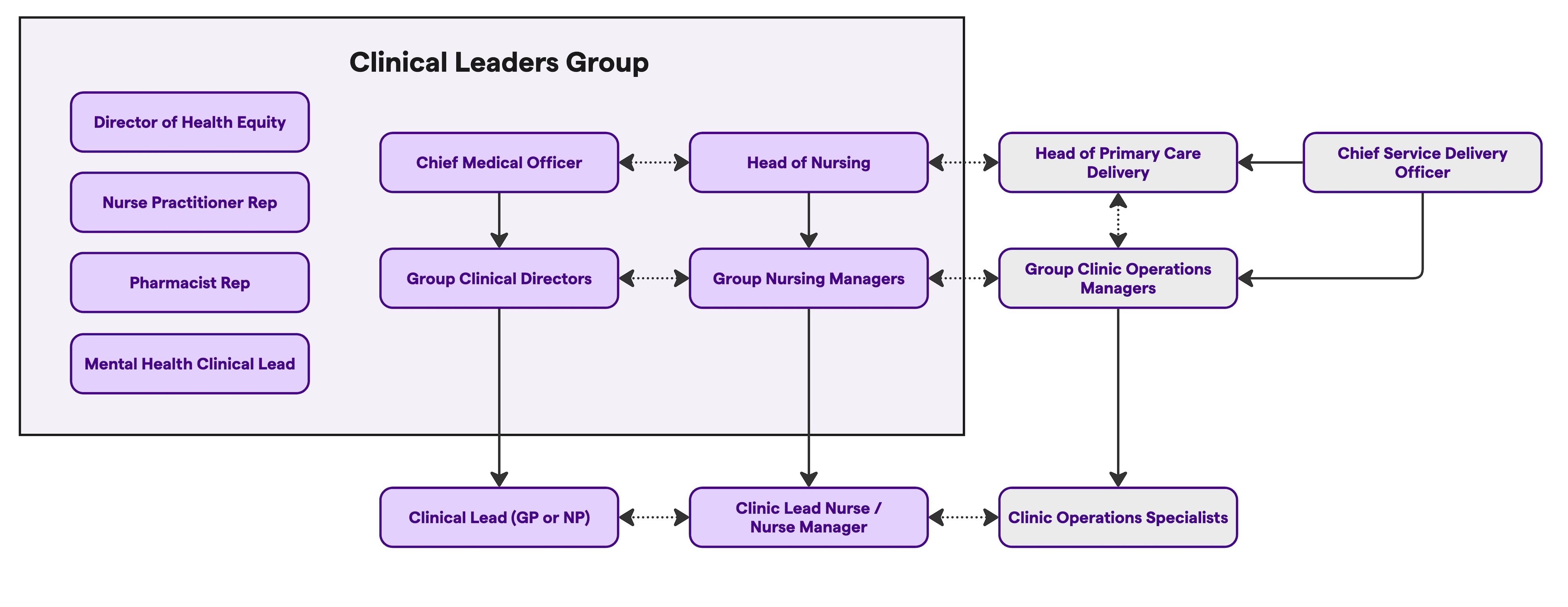
Tend clinical leadership team
At Tend, clinical leadership and governance is GP-led and embedded across our teams and operations to support best-practice, continuous quality improvement, and a sustainable primary care workforce.

Dr Graham Denyer - Chief Medical Officer (CMO)
Member of the Executive Leadership Team and reports to the Board, ensuring clinical risk, patient safety, and quality improvement remain central to organisational decision-making.
Learn more

Nicky Holder - Head of Nursing
Leads nursing workforce development, clinical practice standards and service delivery nationwide.
Learn more
Clinical governance & quality
GP leadership structure
Chief Medical Officer (CMO), who sits on the Executive Team and leads the Clinical Leaders Group (CLG), with formal reporting into the Tend Board. The CMO is responsible for overall clinical direction, quality, and governance.
Group Clinical Directors (GCDs) who are senior RNZCGP Fellow GPs and are responsible for clinical oversight of a regional group of practices and are represented on the Clinical Leaders Group. Note: In future a GCD could also be a very senior Nurse Practitioner.
Clinical Leads who are senior RNZCGP Fellow GPs or senior Nurse Practitioners serving as the primary point of contact for local clinic leadership.
Nursing leadership structure
Head of Nursing (HoN) is the professional lead for all nurse leaders across Tend and is responsible for advancing the national nursing work programme and contributing to all model of care changes / projects. The Head of Nursing sits on the Clinical Leadership Group and is frequently invited to Executive Team meetings to report on progress relating to the nursing programme.
Group Nurse Managers (GNMs) are responsible for leading the nursing teams and services across a group of clinics in a region or area. The Group Nurse Manager formally manages all nursing team members for their clinics and is responsible for the performance, quality, and implementation of the Tend model.
Nurse Leads are the nurse lead for each clinic and are responsible for the day to day delivery of nursing services. They are responsible for rostering and daily workforce management of the nursing team.
Nurse Managers are appointed where we have rural or remote clinics without scale to share leadership across sites.
Clinical leadership group
The Clinical Leaders Group (CLG) at Tend provides clinical governance and leadership to enhance clinical quality and safety, continuous improvement, and health equity.
The group’s primary objectives include:
- Supporting clinical excellence and best-practice to improve patient safety and service quality.
- Driving continuous improvement using evidence and patient feedback.
- Monitoring health equity for Māori and underserved communities.
Specific functions include:
- Improving quality of care by advising on improvement activity and implementing learnings across Tend Health.
- Addressing clinical performance and emerging clinical risks. Promoting evidence-based best practices for continuous quality improvement and service development.
- Monitoring clinical indicators and metrics related to risk mitigation, PHO, and the Tend Outcomes Framework, then advising on actions for improvement.
- Advising on the Tend Model of Care, including systems development and implementation to to improve service quality.
- Increasing opportunities for professional development, well-being, and training to support the workforce.
- Reviewing adverse events/near misses to enhance patient safety.
- Improving health equity through supporting Māori leadership, partnerships, and options for improved access and cultural safety.
- Enhancing care for high needs patients by supporting quality outcomes and safety through technology-enabled care planning and structured pathways.
The Clinical Leadership Group is composed of the senior clinical leadership team, Hauora Māori leadership, and representatives from each clinical role, with regional representation across Tāmaki Makaurau / Auckland, Te Moana-a-Toi / Bay of Plenty and Te Waipounamu / South Island.
Continuous quality improvement
Tend’s Quality Framework integrates real-time data analytics, AI-driven clinical audits, and monitoring of clinical indicators. This enables identification of clinical risks, service improvements, and alignment with best-practice guidelines.
Our clinical audit processes include:
- Routine reviews of clinical notes to assess documentation quality, care planning, and coding.
- Prescribing audits to monitor prescribing practices against best-practice guidelines. For example antibiotic stewardship - the rate of antibiotic prescribing for upper respiratory tract infections.
- Incident and near-miss tracking, ensuring rapid response and learning from adverse events.
Workforce development
A high-quality, well-supported workforce is essential for sustainable primary care. Tend actively supports its clinicians' professional development.
Key initiatives include:
- Peer review groups for case discussions and reflective practice
- Clinical education including student nurse practicums
- Training and resourcing in cultural safety, health equity, and Te Tiriti o Waitangi
- A focus on clinician wellbeing, integrating staff pulse surveys and well-being initiatives into workforce planning
- Clinical supervision and training support for nurses and GPs who are in training or joining from overseas.